Having said that, learning about the degrees of symptoms and current treatments is invaluable to know what to expect and how to live a full life with Parkinson’s.
Why is Parkinson’s Disease Hard to Predict?
Research is ongoing on the causes and progression of PD.
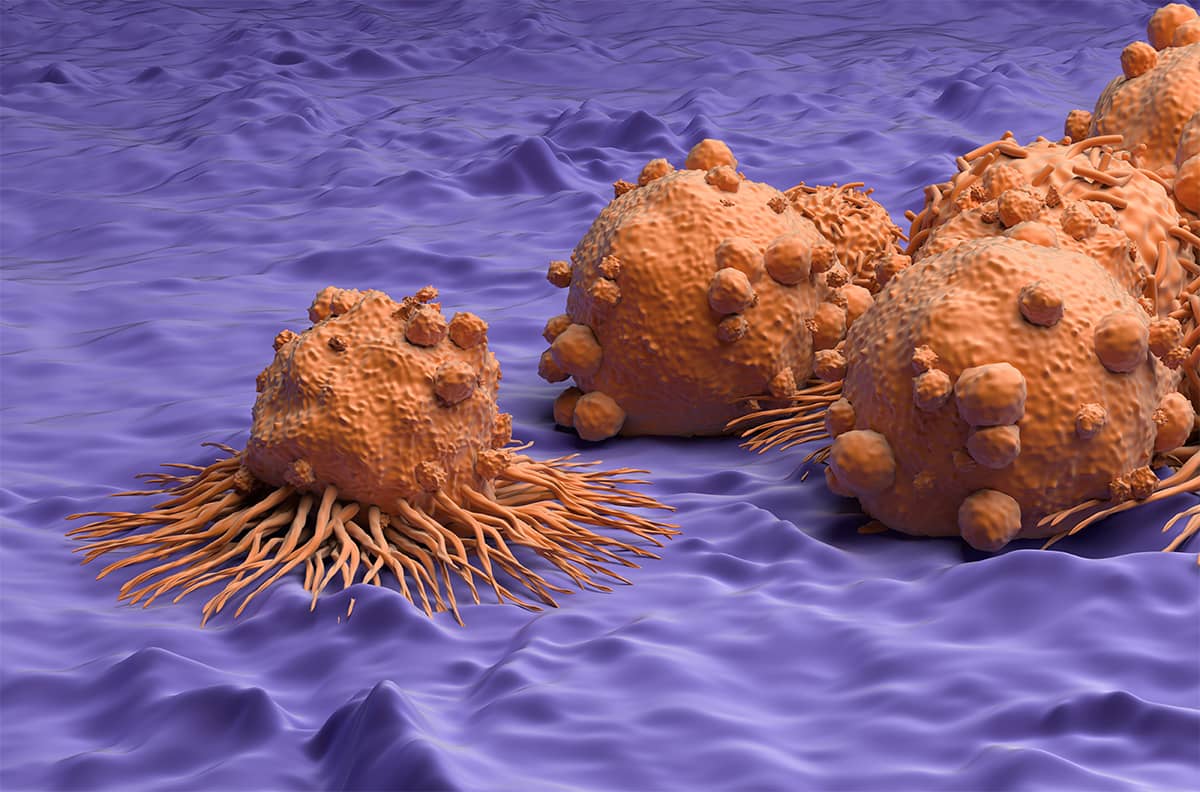
Parkinson’s is a degenerative neurological disorder caused by a protein called alpha-synuclein that accumulates in certain parts of the brain. This results in a progressive decrease in dopamine-producing cells critical to many body functions, such as coordinated movements.
What Are the Causes of Parkinson’s Disease?
While the disease is well-researched, scientists still do not know exactly why these proteins form. However, several factors seem to play a role:
Genetics
Genetics are reported to cause 10-15% of PD cases. Years of studying the DNA of people living with PD has revealed dozens of gene mutations linked to Parkinson’s. Some of these genes are inherited or passed down from generation to generation.
Environmental Triggers
Certain environmental exposures may increase the likelihood of developing PD, while others may even decrease it. For example, they may include head injury, area of residence, or exposure to pesticides, among others.
Diagnosing Parkinson’s Disease
A huge challenge that doctors and the Parkinson’s community face is in diagnosing the disease.
One of the main medical challenges with PD is early identification. Because there is so much symptom overlap between PD and other neurological diseases, it can be difficult to properly diagnose it in its early stages.
Clinical Diagnosis
There is not currently a definitive laboratory test to diagnose PD. Doctors typically diagnose the disease by analyzing a person’s medical history and conducting a neurological exam. This leaves diagnosis largely at the discretion of a clinical professional over months and sometimes years of care and observation.
DaTscan for Diagnosis
Another means of diagnosis is DaTscan testing. This test works by injecting DaTscan, a special radioactive tracer, into the bloodstream. It then travels to the brain and attaches to the molecules that are found on dopamine receptors.
Special imaging equipment is used to scan the head and determine how much DaTscan is present. People with PD typically have a smaller signal in the area of the brain where the dopamine neurons are located.
While a negative DaTscan does not necessarily rule out PD, a positive result can help to confirm it. One advantage is that a positive DaTscan can differentiate PD from essential tremor (ET), which is not characterized by a dopamine deficiency. However, a positive result can also be indicative of other forms of atypical parkinsonism. In summary, a DaTscan can be very helpful in specific scenarios but does not necessarily diagnose PD.
Due to the difficulty in early identification, some people will have lived with PD for years prior to their diagnosis. As such, the stages and symptoms associated with the disease may depend upon where a person is in their care and treatment.
Understanding the Symptoms of Parkinson’s Disease

Generally, two categories of symptoms are experienced with a PD diagnosis. One impacts motor functionality and the ability to move, and the other relates to cognitive symptoms.
Not everyone will experience all of these symptoms, and the severity of symptoms varies on a case-by-case basis. In addition, some of these may occur early in a diagnosis, while others will never materialize.
These are the most frequently observed motor symptoms of Parkinson’s Disease:
- Uncontrollable shaking and tremors
- Slowed movement
- Difficulties with balance
- Stiffness in limbs
Additionally, nonmotor symptoms are just as common, with some people developing them years before they develop Parkinson’s or even years after. These may include:
- Difficulty with memory or planning
- Anxiety and depression
- Loss of sense of smell
- Insomnia
- Fatigue
- Constipation
- Vision problems
- Difficult swallowing
- Speech problems
Gastrointestinal (GI) issues have traditionally gone under the radar. Still, there is a renewed interest in studying the relationship between gut health and Parkinson’s disease due to its significant impact on people’s lives. In addition to the above list, it is not uncommon to experience diarrhea, bloating, heartburn, and fluctuations in weight.
Theories on Parkinson’s Disease Stages

Even without a “one size fits all’ approach to diagnosis, there are years of research that can guide the general trajectory of PD. Regarding motor symptoms, authors like Hoehn and Jahr have attempted to define five main stages of progression.
The Five Stages of PD (The Hoehn and Jahr Scale)
The Hoehn and Jahr scale (named for its authors) was published in 1967 and was the first to describe the progression of PD.
One clear advantage of this rating scale is its simple use. However, this simplicity also leaves something to be desired when accounting for the complexities of PD, its very individualized impact from person to person and the lack of assessment of the cognitive elements of PD.
Doctors utilize this rating system to help evaluate how far the disease has advanced in someone living with PD. Stages 1 and 2 are classified as “early stage,” stages 2 and 3 as “mid-stage,” and 4 and 5 as “advanced stage.”
Note that not everyone living with PD will reach the advanced stages of the disease, with some even only experiencing mild symptoms.
Stage One
This stage is characterized by mild symptoms that do not typically interfere with daily activities. However, they can be so minimal that they are often missed altogether. Symptoms include
- Tremor and other movement symptoms on one side of the body only
- Changes in posture, walking, and/or facial expressions
At this stage, prescription medicine is a highly effective means of mitigating symptoms.
Stage Two
An escalation in Stage One symptoms characterizes this stage. This includes:
- Tremor, rigidity, and other movement symptoms on both sides of the body
- More dramatic changes in walking and posture
- Increased difficulty in accomplishing daily tasks
Progression from Stage One to Stage Two can take anywhere from months to years.
Stage Three
During Stage Three, loss of balance and coordination are more common, resulting in a higher likelihood of falls. Additionally, motor symptoms worsen, and movements become slower overall. While a person may still be able to lead an independent lifestyle, they are somewhat restricted in their activities.
Stage Four
A significant marker of Stage Four is the loss of independence. During this stage, symptoms are fully developed. A person may be able to stand or walk without assistance but require a cane or walker for extra assurance. Symptoms are severely disabling, and the person can no longer live alone without assistance.
Stage Five
This is the most advanced stage. A person may experience leg stiffness that renders them bedridden or confined to a wheelchair, and constant supervision is required. According to the National Library of Medicine, up to 50% of people in the advanced stage of PD experience hallucinations and/or delusions.

The MDS-UPDRS Scale
A major criticism of the Hoehn & Jahr rating system is that it only measures PD in terms of movement. In reality, impairment in motor skills is only one piece of PD. Additional symptoms, such as cognitive impairment, can be significant and impact how Parkinson’s progresses.
Because of this, another rating system is often employed, known as the MDS-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS).
Created in the 1980s, the MDS-UPDRS was refined to address both the impacts on non-motor and motor experiences of daily living.
The assessment consists of 50 questions within four sections relating to both motor and non-motor symptoms related to PD. The four sections are:
- Section 1: non-motor experiences of daily living
- Section 2: motor experiences of daily living
- Section 3: motor examination
- Section 4: motor complications
Within these sections are a series of response forms and questionnaires that analyze symptoms such as cognitive impairment, psychosis (hallucinations/delusions), depression and anxiety, and sleep problems, among others.
There is also a Motor Examination and analysis of Motor Complications. Finally, a final score is formulated based on this series of questionnaires and examinations to give a robust picture of disease progression.
While this system is considerably more complex than the Hoehns & Jahr system, it also gives a more holistic picture of PD progression across a diverse population.
Young Onset Parkinson’s Disease

How Parkinson’s progresses may also depend on when a person is diagnosed. Young Onset Parkinson’s Disease (YOPD), also known as “early onset,” occurs in people younger than 50 years old and is relatively uncommon.
According to 2020 data, 3–5% of people experience YOPD before age 40. While highly uncommon, symptoms of YOPD can start to appear in a person as early as their 20s or 30s.
People with YOPD will experience similar motor symptoms to those with PD. However, they tend to exhibit cognitive issues less frequently. They also tend to have a slower progression of the disease over time.
While the symptoms of young-onset Parkinson’s disease are similar to those later in life, the journey to diagnosis can be significantly different.
Younger people may need to see multiple doctors before finally receiving a correct diagnosis. Doctors aren’t necessarily looking for YOPD or have the experience to address it. As a result, physical symptoms can be incorrectly attributed to sports injuries or stress and anxiety. In such cases, prescribed medications seldom address the underlying condition.
The main difference with younger people living with PD is that the progression of the disease is generally slower over time. Other differences include:
- Less common to experience cognitive issues like dementia
- More likely to experience dystonia, a neurological condition that causes muscles to contract and spasm involuntarily
- More likely to experience dyskinesia, a condition characterized by involuntary movements as a side effect of long-term levodopa use
Young-onset Parkinson’s can have a greater impact on a person’s life, as it can alter your relationship with work, family, money, school, and social activities.
For young people with Parkinson’s disease, it is important to seek a doctor (along with specialists like movement disorder specialists) who can tailor a treatment plan to meet individual needs and goals is important. Then, with the right support, it’s truly possible to live well with the condition.
Treatment and Impact on Progression of Parkinson’s Disease

Following a diagnosis, consulting with a movement disorders specialist is the next best step. A movement disorders specialist is a neurologist specializing in diagnosing and treating neurological conditions that affect movement, such as Parkinson’s.
While a regular doctor can provide initial care and medication, a movement disorders specialist can offer more specialized care. For example, a specialist can help create an individualized treatment plan that may include medications, physical therapy, and lifestyle changes.
They can also help manage their symptoms and side effects and provide support and resources for them and their families. In addition, seeing a movement disorders specialist can help ensure a person receives the best possible care and treatment for Parkinson’s.
Different treatment methods and symptom mitigation strategies may impact how a person experiences PD.
Levodopa
Levodopa is considered one of the most potent medications for PD. It is often the first line of defense a doctor will go to when considering treatment and management of symptoms. How someone responds to Levodopa will impact how their journey with PD develops.
Levodopa is often used in conjunction with Carbidopa to reduce symptoms of nausea and vomiting. In pill form, it works by traveling to the brain via the small intestine, where it is converted into dopamine. This supplementation of dopamine is critical as it aids in daily motor functions such as dressing, walking, and handling utensils.
Studies are inconclusive on whether or not Levodopa slows the progression of PD. In a 2019 study, research suggested that while Levodopa may not necessarily slow the progression of PD, it is safe to take in early stages of the disease. In fact, doing so helps manage typical symptoms and maintain a more pleasant quality of life.
Surgical Treatment
Surgical treatment is typically only explored for those who cannot manage their symptoms with medication. There are two primary forms of surgical treatment: Deep Brain Stimulation (DBS) and Duopa.
Deep Brain Stimulation
DBS works by inserting electrodes into a targeted area of the brain. An impulse generator battery (known as an IPG) is then placed under the collarbone or in the abdomen to deliver an electrical stimulation to targeted areas of the brain.
After undergoing DBS, most people with PD will still need to take medication. However, many people experience a reduction in their PD symptoms and a subsequent increase in their quality of life.
Duopa
Duopa is a form of Levodopa-Carbidopa that delivers the medication directly to the intestine in gel form. This is achieved by making a small hole (a “stoma”) in the person’s abdomen to funnel a tube to the intestine and then using a pump to deliver the gel.
Duopa eases symptoms in an identical way to Levodopa treatment. It may not slow the progression of the disease, but symptoms are easier to manage.
Physical & Speech Therapies for Parkinson’s Disease

Incorporating a combination of therapies into a person’s routine may improve or alleviate common symptoms of PD.
Physical Therapy, including gait and balance training, resistance training, and regular exercise, is proven to help with balance, posture, pain, and general mobility.
Speech Therapy is key to boosting communication skills and confidence. Research shows that up to 89% of those with PD experience changes in speech. This can range from a decrease in volume, reduced clarity, and/or a breathy/hoarse vocal quality, among others.
Working with a speech-language pathologist helps people with Parkinson’s to maintain effective communication as their disease progresses.
Parkinson’s Disease and a Healthy Lifestyle
Recent studies suggest that a powerful antidote to PD may start at home. Incorporating nutritious meals and regular exercise into a daily routine may slow Parkinson’s advancement.
Foods that Aid in Symptom Relief

Overall, doctors recommend a diet of fruits, vegetables, and lean protein to help slow or alleviate the symptoms of Parkinson’s disease. Additionally, those living with PD should monitor their sugar and salt intake and incorporate foods rich in antioxidants. These include anything rich in vitamins C, E, A, and beta-carotene.
A few primary dietary guidelines to note:
- The fiber in fruits, vegetables, beans, and whole grains can help ease constipation.
- Those with high blood pressure should avoid foods with high sodium. Too much salt can be damaging to the kidneys.
- Foods that are sour, seasoned, or carbonated may aid in saliva production, making it easier to swallow.
- Tonic water, pickle juice, and vinegar have been shown to reduce muscle cramping.
- Alcohol should be drunk sparingly, if not removed from the diet, as it can further exacerbate issues with balance and/or health problems unrelated to PD.
Additionally, experts published research in 2022 suggesting that consuming foods rich in flavonoids may help reduce mortality rates in the Parkinson’s community. Flavonoids are antioxidant compounds present in brightly colored food, including:
- Blueberries
- Dark chocolate
- Tea
- Strawberries
Overall, “good food” replenishes essential vitamins and minerals, bolsters healthy living, and protects against harmful environmental factors.
Exercise for Symptom Relief

The Parkinson’s Outcomes Project shows that at least 2.5 hours of exercise per week can slow PD symptom progression and overall decline in quality of life. Additionally, referrals to physical therapy early on in a diagnosis can help prevent hospitalizations and falls.
Incorporating exercise as a regular part of a person’s treatment plan may help to slow the progression of certain motor and cognitive symptoms. Try these at-home fitness options specialized for those living with PD.
Practicing Self-Care
An important part of maintaining a healthy lifestyle is fostering mental health. This includes prioritizing a consistent sleep schedule, keeping in touch with a social network, and making time for hobbies.
As a newly diagnosed person with PD, isolating can be especially harmful to a person’s mental health, leading to anxiety and depression. To counter this, find support groups, in-person sessions, and events to stay connected with people in the PD community.
Additionally, keeping a daily journal can help process emotions around a diagnosis and track symptoms and monitor their progress over time.
While there is not yet one “cure-all” to Parkinson’s Disease, these treatment methods have proven to be effective in managing some of PD’s more difficult symptoms and contributing to an overall increase in the quality of life.
Parkinson’s Disease is Highly Individualized

No one person’s journey with Parkinson’s Disease will look the same as another’s. Some people experience only mild to moderate symptoms of PD throughout their lifetime. Further, symptoms may worsen over many years, if they worsen at all.
Many people go on to live fulfilling lives following their PD diagnosis. A combination of medication, physical and speech therapies, and healthy living is proven to alleviate symptoms and, in certain cases, stave off the rapid progression of PD.
Feel free to reach out to PCLA to get support and resources to help you live a fruitful life and join our thriving PD community.

0 Comments